Initiative seen as easing primary care physician shortage
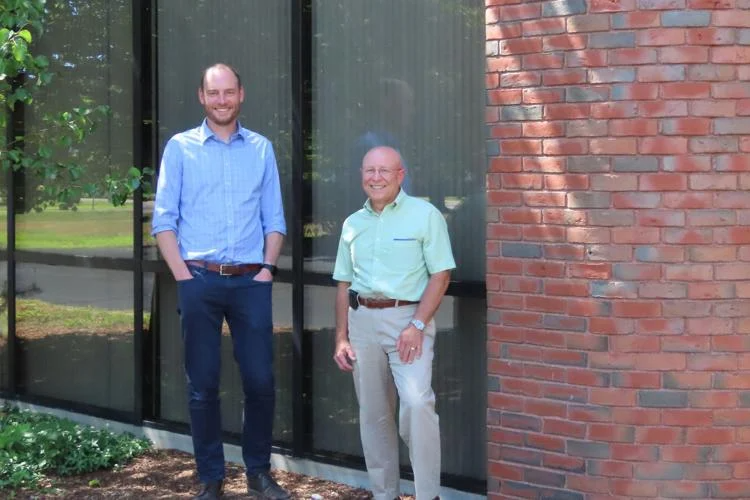
Drs. Karl Dietrich, left, and Christopher LaRocca are leading the effort to develop a family medicine residency at Cheshire Medical Center in Keene. The program recently received a $750,000 federal grant to facilitate its accreditation, with funds also allocated for curriculum design and resident recruitment. (Courtesy Cheshire Medical Center) Cheshire Medical Center in Keene faces a daunting task in working to address the primary care physician shortage in New Hampshire. But the effort just got a little easier, thanks to a $750,000 federal grant that will be used to support the medical center’s family medicine residency program.
The Rural Residency Planning and Development grant from the Health Resources and Services Administration (HRSA) is one of only 11 awarded nationwide this year. It’s designed to help rural institutions attract more newly minted doctors to their programs. The end goal is to improve healthcare access for rural Americans — exactly what Cheshire Medical is hoping to do with its forthcoming residency program.
“HRSA’s goal of improving the health of communities is in line with Cheshire’s vision,” said Dr. Karl Dietrich, program director of the residency.
After finishing college and medical school, new doctors must complete onthe-job training, known as residency. During residency, doctors are supervised by a board-certified physician, but they see patients directly, increasing the number of patients a medical organization can serve.
When the residency is fully operational — hopefully by 2027 — its providers will serve up to 10,000 patients, said Dr. Christopher LaRocca, director of graduate medical education and family medicine residency development at Cheshire Medical. Dietrich is already seeing patients at the medical center on Court Street.
To accommodate the program, the Dartmouth Health affiliate purchased property at 62 Maple Ave. in Keene, the former Peerless Insurance building. The property, which the hospital purchased last May for $4.6 million, encompasses a 147,000-square-foot building and 47 acres of land. There, the residency program will operate a family medicine clinic, distinct from the family medicine department at the hospital’s main campus at 580 Court Street.
Renovations have begun in the area that will be used for the residency program on Maple Avenue, and are expected to be completed in the spring, said Heather Atwell, spokesperson for Cheshire Medical Center.
While some staff for the residency have been hired, the process is expected to continue throughout the winter, she said. However, hiring is on schedule, and staff for the residency — who are themselves healthcare providers — will begin seeing patients at the Maple Avenue location around next July, Atwell said. After that, additional renovations will be considered.
This fall, officials from the Accreditation Council for Graduate Medical Education will visit Cheshire Medical to assess the program. A portion of the grant funds will be used to facilitate accreditation, with funds also allocated for curriculum design and resident recruitment, LaRocca said.
700 programs nationwide
If all goes as planned, the program will be accredited next year and six residents will come to Cheshire Medical in 2024 to begin the three-year program. Six more will matriculate each year, until the residency reaches its full capacity of 18 doctors, LaRocca said.
The value of the residency program isn’t just in bringing more doctors to the state right now. A 2013 research study found that 56 percent of doctors practice within 100 miles of where they completed their residency.
“Our hope is (that) by training more people in rural areas, they get to see all the wonderful parts of living here and working in a community like this, and they are more likely to stay,” Dietrich said.
There are about 700 family medicine residencies nationally, most of them in urban and suburban settings. The two existing family medicine residency programs in New Hampshire, in Concord and Portsmouth, are no exception. Cheshire Medical’s program will offer residents the ability to work with a top-notch medical center — Dartmouth Hitchcock Medical Center — while also experiencing the challenges of providing care in a rural setting, Dietrich said.
Even if the doctors in the residency don’t stay around Keene, they may be more likely to work in rural areas elsewhere.
“Some people who may not want to stay right here, but will still want to stay in rural areas,” LaRocca said. That’s important, too. “This is not a problem unique to this area.”